New technology helps improve organ transplantation – Deseret News
Filed under:
By Jasen Lee
SALT LAKE CITY — New technology in organ harvesting could save the lives of ailing patients in dire need of liver transplants.
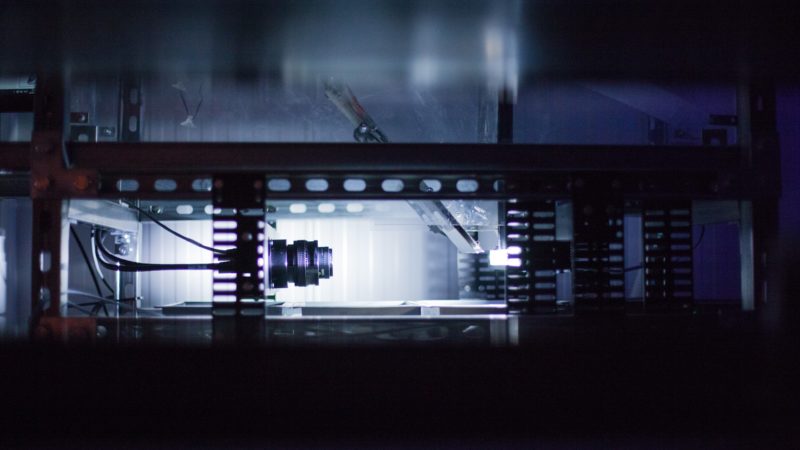
Using new state-of-the-art technology that preserves donor organs by keeping them cold and healthy during transportation for lifesaving surgery, doctors at Intermountain Healthcare have performed the first liver transplants with it in the Beehive State.
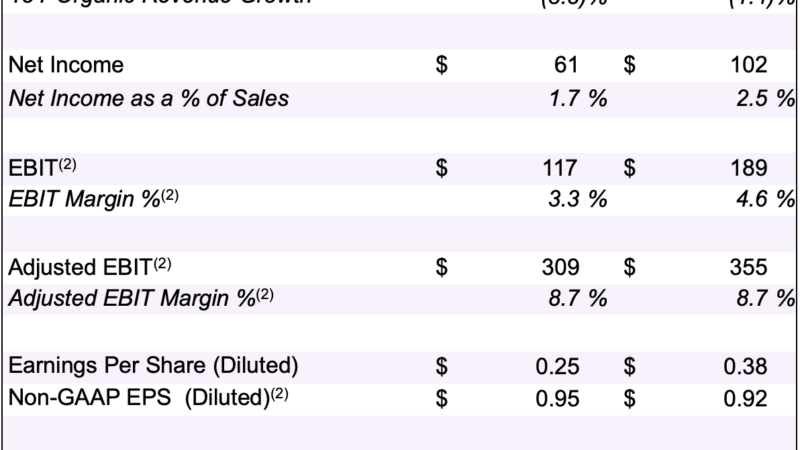
The organs were preserved using portable hypothermic machine perfusion, which circulates a specially formulated, cold medical solution into a donated liver situated inside a machine pump while the organ is taken from the donation point to the awaiting recipient who is prepared for transplant surgery, according to Intermountain officials.
Previously, liver organs have been transferred from one site to another using “static” cold preservation — placing the liver in a solution inside an ice-filled cooler. The new “active” preservation method is designed to enhance the standard technique, which has been in use since 1967.
Thus far, the transplant research team has used the device in 10 procedures in conjunction with a multicenter clinical trial that compares the traditional cold storage method of organ transportation to the portable hypothermic machine preservation system.
“The primary objective of this study is to collect clinical data to provide reasonable assurance of safe and effective use of transporting livers for our transplant patients,” said Dr. Diane Alonso, program director of Intermountain Healthcare’s abdominal transplant program and principal investigator on the clinical trial.
“In the long run, we hope to use this technology in the future to increase the number of organs available for transplantation, while reducing complications and shortening the length of hospital stays.”
She said the new technology may allow transplant teams to condition donated livers or assess potential donor livers in a better way to determine if they can actually use organs that otherwise would have been discarded.

“(Also), we can transport these organs from further distances because they can survive on the pump longer and that expands our organ pool and every organ counts because that has one more life saved,” Alonso said.
“If we can expand the pool by 5% or 10%, that’s a big deal. That’s a really big deal!”
Intermountain surgeons perform approximately 50 liver transplants annually, she said, with between 140 and 150 patients on the waiting list at any given timed.
Each year, an estimated 2,500 patients die in the U.S. while on the liver transplant waiting list. With viable organs in short supply and less than 60% of American adults registered as organ donors, this new device could help more patients become recipients, explained Jake Krong, Intermountain Healthcare transplant research operations manager.
“There’s a need now with so many patients listed for transplant,” he said. “We want to be able to use every organ that’s available out there to get it transplanted into somebody who needs it.”
Typically, organs can remain viable for about 12 hours after removal from a donor, according to Jake Finnerty, surgical recovery coordinator with DonorConnect.
“Hopefully what this will do is make those organs much more viable, much more ready to transplant and really boost the number of livers that we can get out to people on the list,” he said.
DonorConnect and Intermountain Healthcare are currently involved in a clinical trial that could determine whether machine perfusion improves overall outcomes for transplant recipients, according to a statement from Intermountain. The long-term goal is for the technology to assist transplant centers identify more viable livers for transplant and help bridge the gap between demand and supply, Krong said.
Intermountain is one of five transplant centers actively participating in this clinical trial. The Intermountain Transplant Research Department is collaborating with DonorConnect, Utah’s organ procurement organization, which facilitates and coordinates for donors and donor families throughout the Intermountain West, the statement says.
During the study, DonorConnect organ preservation technicians work with transplant surgeons to connect donated livers to the machine, help transport the livers for transplant, then assist the Intermountain researchers with data collection.
About 140 patients are expected to be enrolled in this randomized trial across the United States in the next year, Krong said. Half of the patients who consent to participate in the research study will receive a liver preserved with traditional static cold storage, with the others receiving machine-preserved organs.
“This collaborative study provides Intermountain patients with access to cutting-edge transplant technology,” Krong said, adding that FDA approval is pending the results of the clinical trial.
“The hypotheses that we have are that (the pump is) going to increase the ability of the liver to start working normally after transplant so the patient should recover faster from their surgery,” he said. “Hopefully we’ll see things like they get discharged from the hospital faster (and) they have fewer complications post surgery. Those are the things that we’re measuring in this study.”
Results of the trial are expected later this year, he said.
West Jordan resident Laura Adams, 47, was among the first patients to benefit from the new technology. When the wife and mother of two was asked if she would participate in the clinical trial, she said, “Why not? You have to see if the pump can help others and it makes perfect sense.”
She was diagnosed with liver cancer last year and was in desperate need of a transplant. A liver match was located, but there was a catch — it was infected with hepatitis C. Doctors told her, “We can cure hepatitis C, we can’t cure cancer.” So she decided to accept the hepatitis C-positive liver.
Today, she has no signs of hepatitis C and is looking forward to a future with her family.
“I kind of feel like I won the lottery,” Adams said. “(My) liver numbers have been perfect consistently — since day one. It feels amazing!”