Consolidation, labor shortages, new technology impacting health care industry in 2023 – BizTimes Milwaukee
This advertisement will close in seconds…
The year 2022 was a big one for merger and acquisition activity among hospitals and health systems in Wisconsin. To understand how the health care marketplace is being transformed by this and other trends – including higher costs, labor shortages and the shift to digital – BizTimes Milwaukee asked several key leaders in the industry to share their observations and forecasts for 2023.
Consolidation continues as costs climb
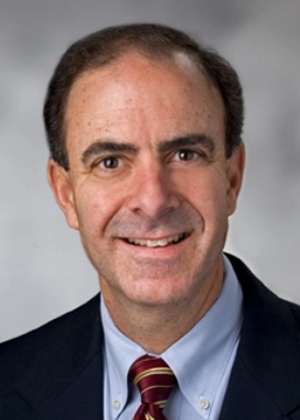
“If we take a look back at the last decade, one of the major changes that occurred was an acceleration of consolidation,” said Bill Santulli, president of Advocate Health’s Midwest region.
There have been approximately 1,519 hospital mergers in the past 20 years, with more than 680 since 2010, according to a 2018 statement before the Committee on Energy and Commerce Oversight and Investigations Subcommittee in the U.S. House of Representatives.
Which leads to recently, when, on Dec. 1, 2022, La Crosse-based Gundersen Health System and Green Bay-based Bellin Health completed a merger. The next day, Milwaukee- and Chicago-based Advocate Aurora Health completed its merger with Charlotte, North Carolina-based Atrium Health. Together, those mergers will impact about 8.5 million patients across several states.
“Fundamentally, both Advocate Aurora and Atrium are legacy organizations, and we believe in scale,” Santulli said. “When we created Advocate Health, we were able to successfully create financial synergies.”
Why hospitals consolidate depends on a variety of factors, but it often comes down to size and scale, which in turn greatly affect the ability of the system to keep costs down, said Brian Potter, vice president of finance and the chief operating officer of the Wisconsin Hospital Association.
“When you’re smaller and trying to wrestle with these challenges, you start thinking about working individually versus together. There’s efficiency in that,” Potter said.
Put simply: the bigger the hospital system, the bigger its support system will be, which is important in cost-cutting and modernization efforts.
When it comes to the latter, geographic location can determine who merges with who and why, Potter said. For example, if a hospital in a rural region is advanced in offering telehealth due to the spread-out nature of its population, that could be an attractive feature for a hospital in an urban area to adopt.

Cost-cutting and modernization efforts have been more of a priority in the past 12 months, as hospitals’ financials have “forced people to seek cover,” said Cathy Jacobson, chief executive officer of Wauwatosa-based Froedtert Health.
“Even pre-financial distress, these mergers are much more about how you build capabilities. How do you put your organization together to create scale and attract talent on a national basis? How do you form tech partners? You need to have a certain scale to be able to participate in that,” Jacobson said.
Froedtert “continues to talk to partners all the time” about the nationwide trend of mergers and acquisitions, Jacobson said. In 2018, Froedtert purchased the former Wisconsin Heart Hospital property from Ascension Wisconsin, and in 2022, Froedtert & the Medical College of Wisconsin partnered with Neenah-based health provider ThedaCare for specialty services.
“The merger conversations aren’t done, and in fact I think they’re going to accelerate due to financial distress,” Jacobson said.
Continued merger conversations have sparked concern among providers and policymakers alike that the result of such actions is a costly and inefficient market that puts consumers at a disadvantage.
“How can you gain efficiency through aggregating your back office? We as an industry have been woefully inadequate in proving our efficiencies,” Jacobson said. “But people continue to merge based on that premise.”
The more health care acts like any other industry, the more patients and communities will suffer, said state Sen. Chris Larson, who provided an example in the case of Ascension recently closing labor-delivery services at St. Francis Hospital in Milwaukee.
“From a business standpoint, you want product delivery to be as efficient and cost-effective as possible. But that means consolidation – it means people traveling farther to appointments, it means fewer providers, it means longer wait times,” Larson said. “The usual incentives that drive innovation in the marketplace don’t apply to health care because patients really aren’t free to shop around, and they can’t withhold their purchase if they don’t like the deal they’re being offered. If you’re sick, you do whatever it takes to get help and deal with the consequences later.”
Jamie Lucas, executive director of the Wisconsin Federation of Nurses and Health Care Professionals, echoed that statement, noting that health care is the largest source of debt for Americans, and although the U.S. spends more than other countries on health care, it generally does not get better results.
“Whose lives are saved is a question of where resources are allocated,” Lucas said, referencing studies that show hospital consolidation has not led to either improved quality or reduced costs.
Labor shortages
The COVID-19 surge in the fall of 2021 hit health systems like a “gut punch,” Jacobson said.
“We really started to see (employees) leave in droves, and we started to see a lot more turnover,” Jacobson said.
Hospital employment is down approximately 100,000 from pre-pandemic levels, according to data from the Bureau of Labor Statistics. Additionally, hospital labor expenses per patient through 2021 were 19.1% higher than pre-pandemic levels in 2019.
“(To my team I say) ‘Tell me what we need to do better, and don’t tell me we need to hire more people, because there aren’t new people to hire,’” Jacobson said. “These shortages are going to be pervasive for the next few years.”
Unlike other industries, such as hospitality where restaurants can limit their tables or hours of operation, or manufacturing where contractors can turn down orders, health care systems must serve demand. Subsequently, due to workforce scarcity, hospitals must pay higher rates for overtime and contract staffing agencies.
“Labor costs tend to be 50%-55% of our expenses, so it is our single biggest cost,” which means any increase on these costs can significantly impact total expenses and operating margins, Jacobson said.
The trend of workforce challenges had begun before the pandemic, Santulli pointed out.
“With the aging of baby boomers, we are not replacing the folks that are exiting the workforce at an appropriate rate,” Santulli said.
Moreover, the supply chain issues that continue to affect every industry are also hitting hospitals. Medical supply expenses grew 20.6% through the end of 2021, compared to pre-pandemic levels. When focusing on hospital departments most directly involved in care for COVID-19 patients − ICUs and respiratory care departments − medical supply expenses increased 31.5% and 22.3%, respectively, from pre-pandemic levels, according to the Bureau of Labor Statistics.
“We need to seriously evaluate whether we’re getting our money’s worth with the way we fund health care in this country,” Larson said, adding, for example, in Wisconsin last year, hospitals reported $2 billion in community benefits, with $1.2 billion being used as write-offs for the difference between the cost of care and the Medicaid reimbursement rate. “Who do you think really makes up the difference? Every other patient who pays out of pocket or with private insurance. So really, we have a system that doesn’t work for anybody except for drug companies and device manufacturers, and a few hospital executives. That’s not sustainable.”
Both Froedtert and Advocate Health have local partnerships to grow their commitment to graduate medical education and health research. But part of the labor shortage problem is the prohibitively expensive cost of education for many people, Larson said.
“We ought to work toward a state and a nation that truly values and invests in lifelong education, to the point where nobody ever has to go into debt to pursue their dreams,” Larson said.
“Going forward, we’re going to have to get innovative in dealing with these challenges, like providing more flexible scheduling and doing a better job at leveraging technology,” Santulli added.
Digital transformation and technology adoption
When it comes to leveraging technology, there are a variety of factors at play, but they are all contingent on support systems that can be built to make providers more attractive as potential partners, Jacobson said.
“You’re going to start to see hospitals making moves to separate themselves from everyone else because the (digital transformation) investments are starting to pay off,” Jacobson said. “It’s going to show a demonstrable difference in terms of experience and engagement.”
Those investments include big data and artificial intelligence. Big data aggregates information through social media, online and financial transactions. For hospitals, patient record analysis using big data could help to estimate future admission rates for accurate staffing purposes, flag inconsistencies between a patient’s health and drug prescriptions and create plans for preventive care. Meanwhile, the health care-AI market – which can be observed in virtual health assistants and precision medicine, among others – is expected to exceed $34 billion by 2025.
“Real digital transformation in my eyes enables patients to interact with health care like they interact with anything else,” Jacobson said. “Whether it makes transactions like paying bills much, much faster, all the way up to how you interact with your doctor virtually, I think health care is just in the early stages of this. How do we use digital tools to engage our patients in a different way?”
On the topic of tech, another significant trend is the shift in the place or venue where care is delivered, Santulli said.
“We’ve seen a shift from acute patients being served in hospitals, to clinics and ambulatory settings, to the home and now to the virtual, and I think this will continue to accelerate this year,” Santulli said.
In 2022, inpatient activity at Advocate Health was down approximately 7%, while outpatient activity increased substantially, Santulli said.
“That does put a lot of financial pressure on us, because traditionally you get reimbursed more in a complex acute environment versus an ambulatory environment,” Santulli said.
But to Larson and his constituents, telehealth has the potential to greatly expand access to care, particularly mental health care, to people who may not have had access otherwise, he said.
“The interstate compact Wisconsin recently joined will allow people a much wider variety of therapists to choose from and could improve cultural competency by allowing people to choose providers with similar cultural backgrounds to themselves,” Larson said.
The next 12 months could bring more digital transformation, along with more challenges, to the health care industry in Wisconsin.
“There’s no silver bullet for any of these things,” said Potter. “Health care just continually changes.”
“2022 was one of the most fiscally challenging years for hospitals and health systems,” Santulli added. “The outlook for this new year is no different.”